Barton Associates 2021 Client Telehealth Survey Report

Introduction
Barton Associates is a locum tenens staffing agency providing physician, nurse practitioner, physician assistant, dentist, and CRNA coverage to multiple different facility types across all 50 U.S. states including but not limited to hospitals, private practices, dental offices, corporate clinics, and IHS facilities.
In Barton Associates’ 2021 Client Telehealth Survey, we set out to gauge facility adoption and usage of telehealth in hopes of providing insight into telehealth usage and trends in 2022 and beyond. Our survey of 230 staffing managers and facility administrators across the country explores how facilities utilized telehealth in 2021, and what benefits or obstacles telemedicine posed for their departments and the patients within them.
Takeaways from the survey indicate that despite staffing managers’ and administrators’ perceived obstacles to adopting or maintaining the usage of telemedicine, that this form of clinical care will likely prevail throughout 2022 and the foreseeable future. This is indicated by 64.1% of those surveyed who said their organization’s leadership is motivated to increase the use of telehealth in their facilities.
2021 Client Telehealth Survey Report details:
-
Facilities’ 2021 general telehealth usage and trends
-
Staffing managers’ reported benefits of the utilization of telehealth in patient care and across their facility’s departments
-
Staffing managers’ anticipated and perceived barriers to patients’ and their organization’s usage and maintenance of telehealth
- Future outlook and predictions for telehealth following the initial COVID-19 surges
How Facilities Utilized Telehealth in 2021
Of the 230 staffing managers and administrators surveyed, more than half (56.5%) indicated that their facility offers telemedicine visits to patients, with 73.7% of those facilities having utilized telehealth for over 12 months.
Most facilities accessed telehealth via Zoom (45.9%) and audio-only telephone (25.6%), with 64.7% of facilities utilizing a combination of different platforms. A large majority of health care providers, 90.2%, conducted telehealth visits at the facility, out of which 38.6% had the option to conduct the visits either at the facility or at their home.
The top three types of visits that facilities offered to their patients via telehealth were for Mental and Behavioral Health (56.5%), Medical Management (55.7%), and Chronic Disease Management (39.7%).
Telehealth Offers Clear Benefits For Facilities Across Their Departments
Our survey found that telehealth is a tool that is not only easy for facilities to learn to use, but that its implementation presents opportunities for improvement across departments. 66.4% of survey respondents reported that it has been easy for them to use telehealth in the departments at their facility, and an astounding majority of respondents (80.9%) agree that telehealth has improved their departments.
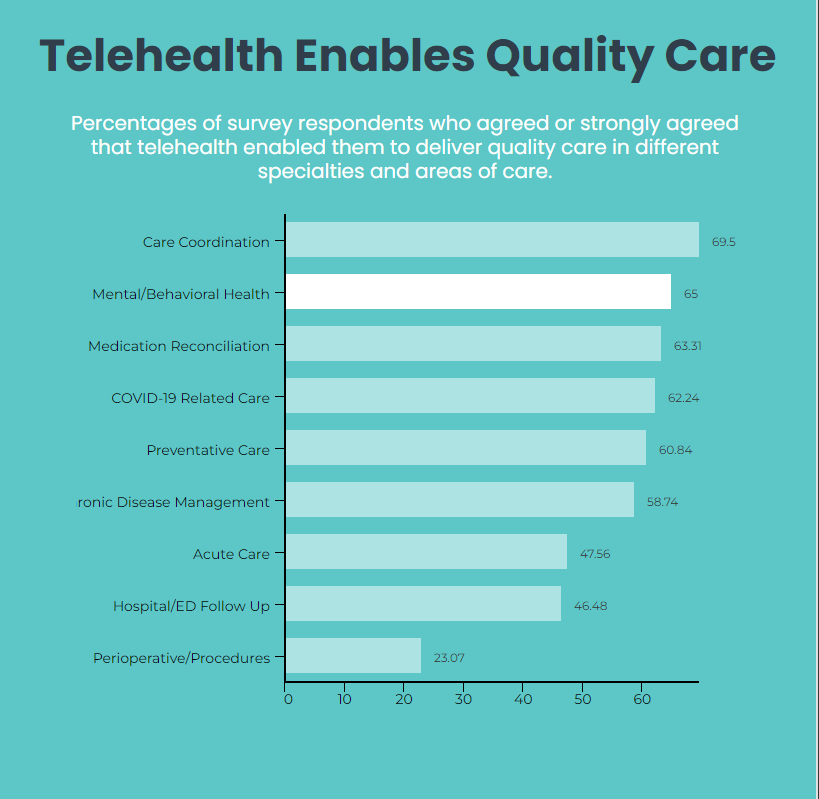
A majority of staffing managers agreed or strongly agreed that telehealth improved both the timeliness of care (58%) and the quality of care (61.2%)*(Figure 1) for patients within their facility’s departments. Interestingly, we found that 55% of staffing managers reported that the departments across their facility average 11+ telehealth visits per week, 38.2% of which reporting an impressive average of 20+ visits per week.
It’s clear to see that telehealth enables providers to see a much higher number of patients per day and devise how this translates into improvement in the timeliness of care for patients ‒ but it also poses the question: How does telehealth improve the quality of care for patients with providers balancing such a heavy workload?
One hypothesis is that telehealth reduces provider burnout, and burnout has been proven to have negative effects on providers’ ability to provide quality care.
As previously stated, the bulk of staffing managers said they are accessing telehealth at their facility using Zoom (45.9%) or audio-only telephone (25.6%), and that 48.5% of facilities allow providers to conduct telehealth visits from their homes. It’s possible that the convenience of conducting visits via telehealth reduces providers’ stress levels, enabling them to focus more on the quality of care they are providing to patients.
Improvements in Facility Departments are Positively Correlated with Improved Patient Wellbeing
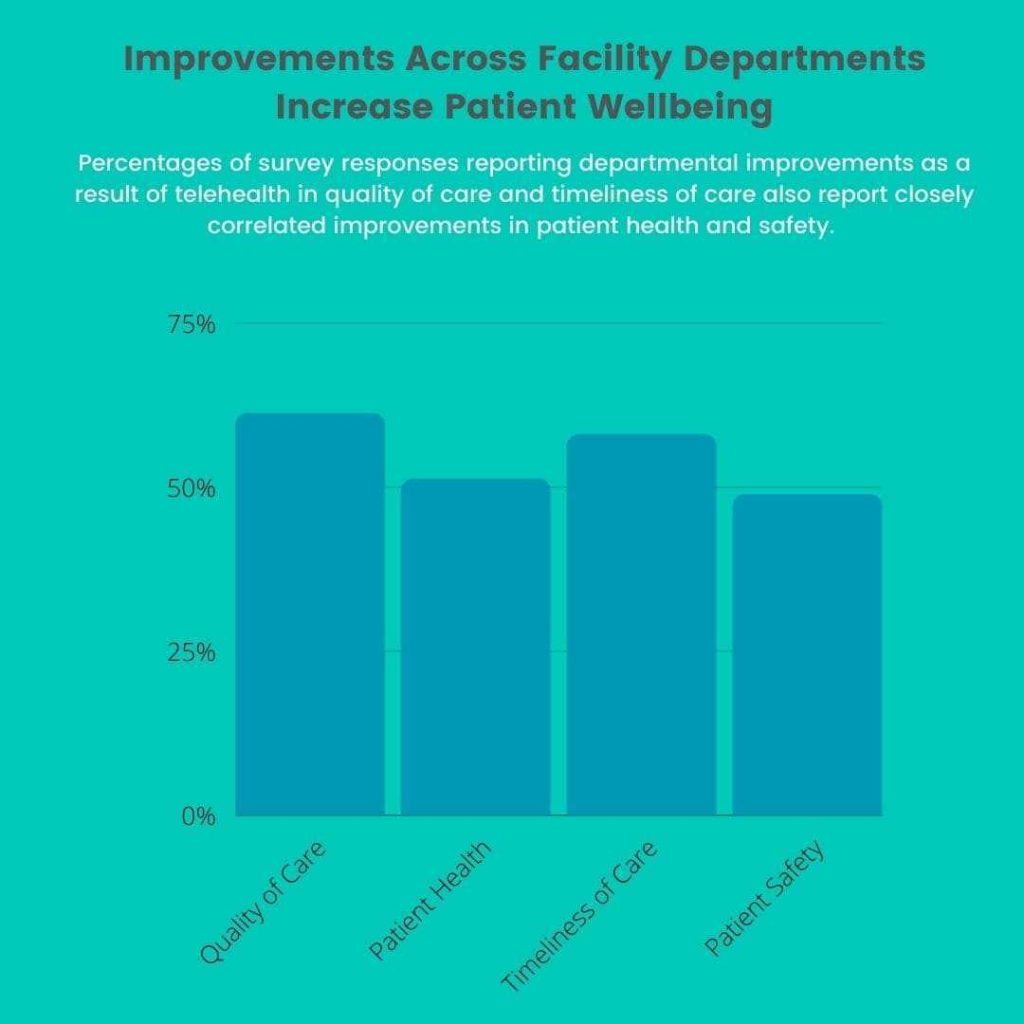
The departmental improvements of timeliness and quality of care are not only beneficial for the facilities themselves, but also trickle down to patients, enhancing their overall health and safety.
As defined by the World Health Organization, quality of care is “the degree to which health services for individuals and populations increase the likelihood of desired health outcomes”. As this definition suggests, quality of care is directly correlated with patient health, which is reflected by our survey results with more than half of respondents (51.2%) reporting improvements in their patients’ health.
Furthermore, as 48.8% of respondents also said that telehealth has improved the safety of their patients, we hypothesize that timeliness of care is correlated with patient safety. Our speculation is that the convenience of telehealth for providers makes them more readily available to patients. This increase in provider availability translates into an increased capacity for them to schedule urgent telehealth visits and address emergency patient issues, therefore decreasing the likelihood that said issues will hurt the patient’s safety.
Our respondents evidently saw the benefits of telehealth for both their facilities and their patients *(Figure 2), and it seems that patient reactions to telehealth were just as positive. When staffing managers were asked how their patients reacted to the telehealth options in their departments, 56.6% of respondents agreed that their patients have reacted favorably to leveraging telehealth for clinical care.
It is interesting to note that most of the remaining responses did not necessarily disagree (7.6%) with the statement, but were instead neutral (26.7%), suggesting that the other portion of respondents may simply not have enough exposure to patients to form a full picture of their reactions to telehealth.
Staffing Managers are Unsure About the Future of Telehealth at Their Facilities
With all benefits to facilities and public health considered, it makes sense that 64.1% of staffing managers reported that their organizations’ leadership is motivated to increase the use of telehealth at their facility. Staffing managers themselves are almost as excited about telehealth, with 52.7% of respondents reporting that they are personally motivated to increase the use of telehealth at their facilities.
Though both leadership and staffing managers across the organizations surveyed seem generally enthusiastic about utilizing telehealth at their facilities, a large percentage (42%) *(Figure 3) of respondents said they were unsure whether or not their organization was planning on using telehealth in 2022.
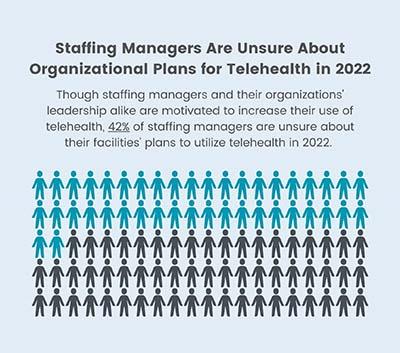
One theory for this inconsistency could be that client managers were simply not involved in the discussion about their facilities’ future plans for telehealth, which, for those surveyed whos’ facilities did not use telehealth, was one reported cause why staffing managers were left in the dark about their facility’s decision.
However, a more plausible cause for this uncertainty may be due to staffing managers’ anticipated and perceived barriers for patients.
54.2% of respondents reported that they anticipate technology challenges for patients being the largest barrier to their organization’s using or maintaining of telehealth, and 57.3% said they perceived lack of patient access to technology, such as computers and smartphones, as barriers to their patients accessing telehealth. We deduce that staffing managers are unsure about their organization’s 2022 plans for telehealth because they are also unsure about patients’ ability to access it.
Contrarily, when asked if they feel that patients at their facility have better access to care since their practice began using telehealth, 64.1% agreed that telehealth actually improved patient access.
As most patients are reportedly accessing telehealth by audio-only telephone calls (50.4%) or by live, interactive video visits at their homes (78.63%), we suggest that, similarly to our conjecture that telehealth is convenient for providers, telehealth improves patient access to care because it’s convenient, and easy for patients to use. The assumption discussed above that telehealth increases provider availability also corresponds to the convenience of utilizing telehealth for patients, as they have better access to care where and when they need it.
If patient access to or difficulty using telehealth technology aren’t an obstacle for organizations’ usage and maintenance of telehealth, then what is?
Further Integration of EHR with Telehealth Technology is Needed
The second biggest barrier to their organization’s using or maintaining of telehealth that staffing managers anticipated was little to no reimbursement for the services rendered (32.1%).
So why are providers not being reimbursed for their telehealth services? Interestingly, while most organizations are accessing telehealth at their facility through Zoom or audio-only telephone calls, 57.9% of respondents say that EHR is integrated with their telehealth technology. Our hypothesis for why providers are not being reimbursed for their services is that their organization’s EHR systems are not properly configured or integrated with the telehealth technology they are utilizing.
With improperly integrated and configured EHR systems, providers are probably not only untrained in combining the two technologies, but are likely spending unpaid time completing charting outside of their scheduled telehealth visits. Those providers utilizing Zoom and telephone calls for telehealth visits likely take notes during the calls, and complete their charting afterwards. Our belief is that providers using this system are only being reimbursed for the time of the telehealth visit, not for the additional time it takes to complete their charting, therefore affecting billing negatively.
Conclusion
Though staffing managers and organizational leadership are inclined to increase their use of telehealth, they were unsure about their telehealth usage plans for 2022. This uncertainty is largely credited to the perceived obstacle of patient access to and ability to use the technology required, despite staffing managers’ reports that telehealth actually increased their patients’ access to care.
Our findings point to another potential barrier to organizations’ use and maintenance of telehealth; low or no reimbursement for services rendered due to unsatisfactory integration or EHR systems with the telehealth technology facilities are using.
Telehealth is not only easy and convenient to use, but improves facilities across their departments, as well as patient outcomes and satisfaction. Due to the evident advantages that telehealth offers patients and facilities alike, our prediction is that the use of telehealth will not only prevail after the end of the COVID-19 pandemic, but for the foreseeable future. In order to continue its prevalence, more commonly used telehealth technologies must improve to better integrate with EHR so charting and billing runs more smoothly for providers.