
Patients today are increasingly willing to use virtual care and telehealth services, partly because of the convenience and ability to improve access to healthcare. According to a 2017 Virtual Visits Consumer Choice Survey from the Advisory Board, 77% of consumers would consider seeing a healthcare provider virtually. Nearly one in five – 19% – had already seen a provider virtually.
However, the law hasn’t completely caught up to the technology despite the growing interest in telehealth. States have their own laws around telehealth licensing, reimbursement and consent, as well as their own definitions for what constitutes telehealth. It is important for patients and healthcare providers to be aware of the laws in their state before using telehealth services.
What Is Telehealth?
There is no standard definition for telehealth, but it is broadly defined as the use of electronic and telecommunications technologies to deliver clinical healthcare services, patient education, public health and health administration. It is often used interchangeably with telemedicine, though the latter typically focuses on the practice of medicine via remote means. Telehealth includes videoconferencing, remote patient monitoring, and store-and-forward. Mobile health (mHealth) can overlap with telehealth, but the two cannot be used interchangeably because mHealth is delivered exclusively via mobile devices such as smartphones and tablets.
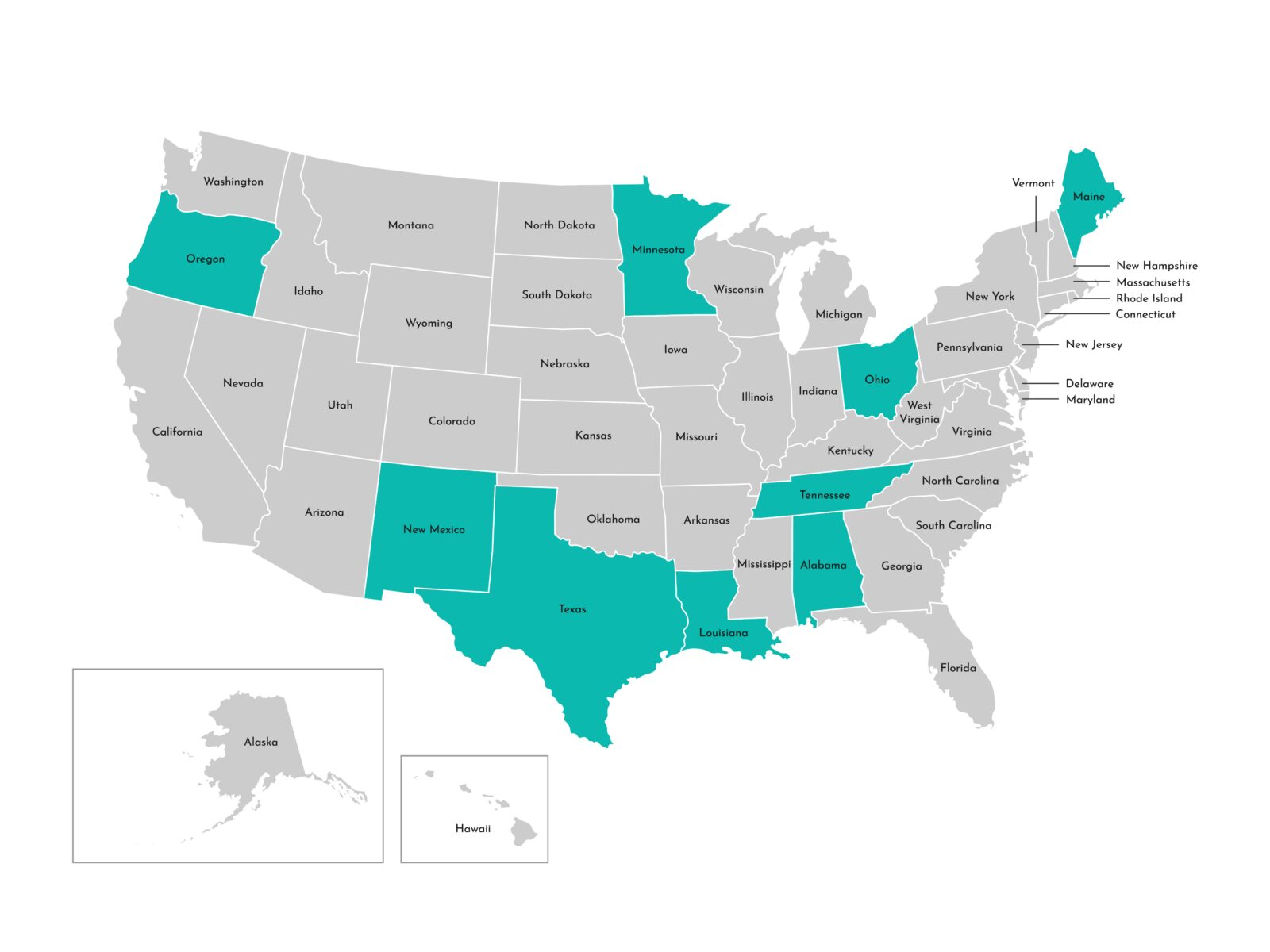
Telehealth Licensing
Licensing for telehealth varies from state to state. According to HealthIT.gov, most states require physicians to be licensed to practice in the originating site’s state, while others require the healthcare provider to have a valid license in the state where the patient is located. In other words, if the healthcare provider is located in Arizona, but the patient is located in Maine, the provider must have a valid license in Maine.
However, progress is being made toward allowing physicians to practice in multiple states. The Interstate Medical Licensure Compact (IMLC) is an agreement between 29 states, the District of Columbia and the Territory of Guam that allows licensed physicians to practice medicine across state lines within the Compact if they meet certain agreed upon eligibility requirements. The Compact expedites the application process by using a physician’s existing information from the state of principal license (SPL).
However, not all states are part of the IMLC yet. For example, Minnesota adopted legislation to enter the Compact in 2015, but must pass two new bills to meet new federal law enforcement background checks requirements, according to the Minnesota Medical Association. New Jersey introduced Compact legislation in May 2019 but is not a member state yet.
Read here to learn more about the IMLC member states that are currently processing SPLs and issuing licenses, those that have delayed implementation, and states that are not members yet.
Further, according to the Center for Connected Health Policy (CCHP), there are nine state medical or osteopathic boards that issue special licenses or certificates for telehealth that allow out-of-state providers to deliver services via telemedicine in a state where they are not located or allow providers to deliver telehealth services if certain criteria are met. Those states are:
- Alabama
- Louisiana
- Maine
- Minnesota
- New Mexico
- Ohio
- Oregon
- Tennessee (osteopathic board only)
- Texas
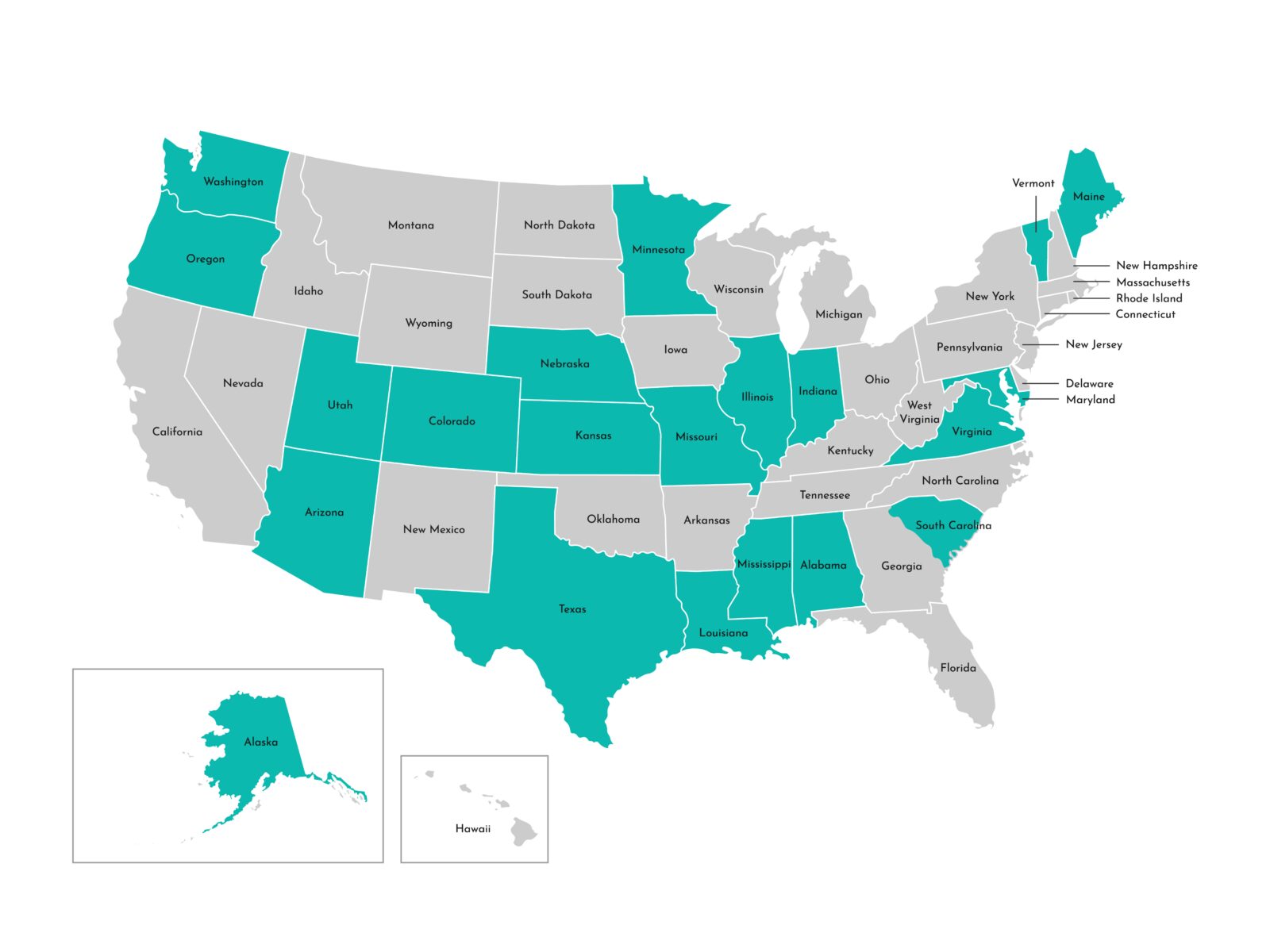
Telehealth Reimbursement
Another area to be aware of when it comes to telehealth is reimbursement. While all 50 states and the District of Columbia provide reimbursement for some form of live video in the Medicaid fee-for-service model, only 21 have some form of reimbursement for remote patient monitoring in their Medicaid programs. Remote patient monitoring is defined as the use of telehealth technologies to collect medical data from patients in one location and electronically transmit that information to a healthcare provider in a different location. The states that offer RPM reimbursement are:
- Alabama
- Alaska
- Arizona
- Colorado
- Illinois
- Indiana
- Kansas
- Louisiana
- Maine
- Maryland
- Minnesota
- Mississippi
- Missouri
- Nebraska
- Oregon
- South Carolina
- Texas
- Utah
- Vermont
- Virginia
- Washington
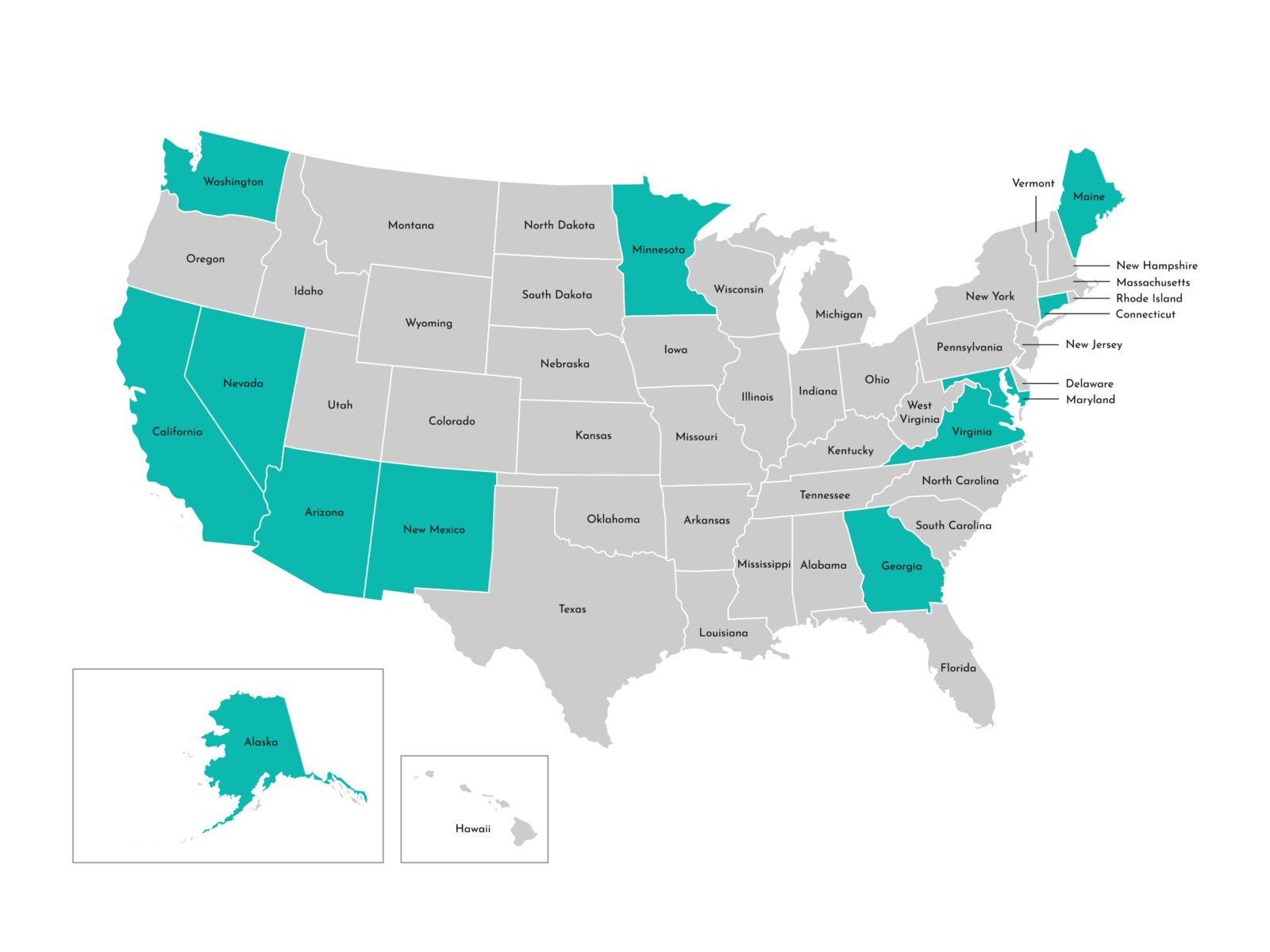
Additionally, only 11 state Medicaid programs include reimbursement for store-and-forward services, which allow for the electronic transmission of medical information such as digital images and pre-recorded videos:
- Alaska
- Arizona
- Connecticut
- California
- Georgia
- Maryland
- Minnesota
- New Mexico
- Nevada
- Virginia
- Washington
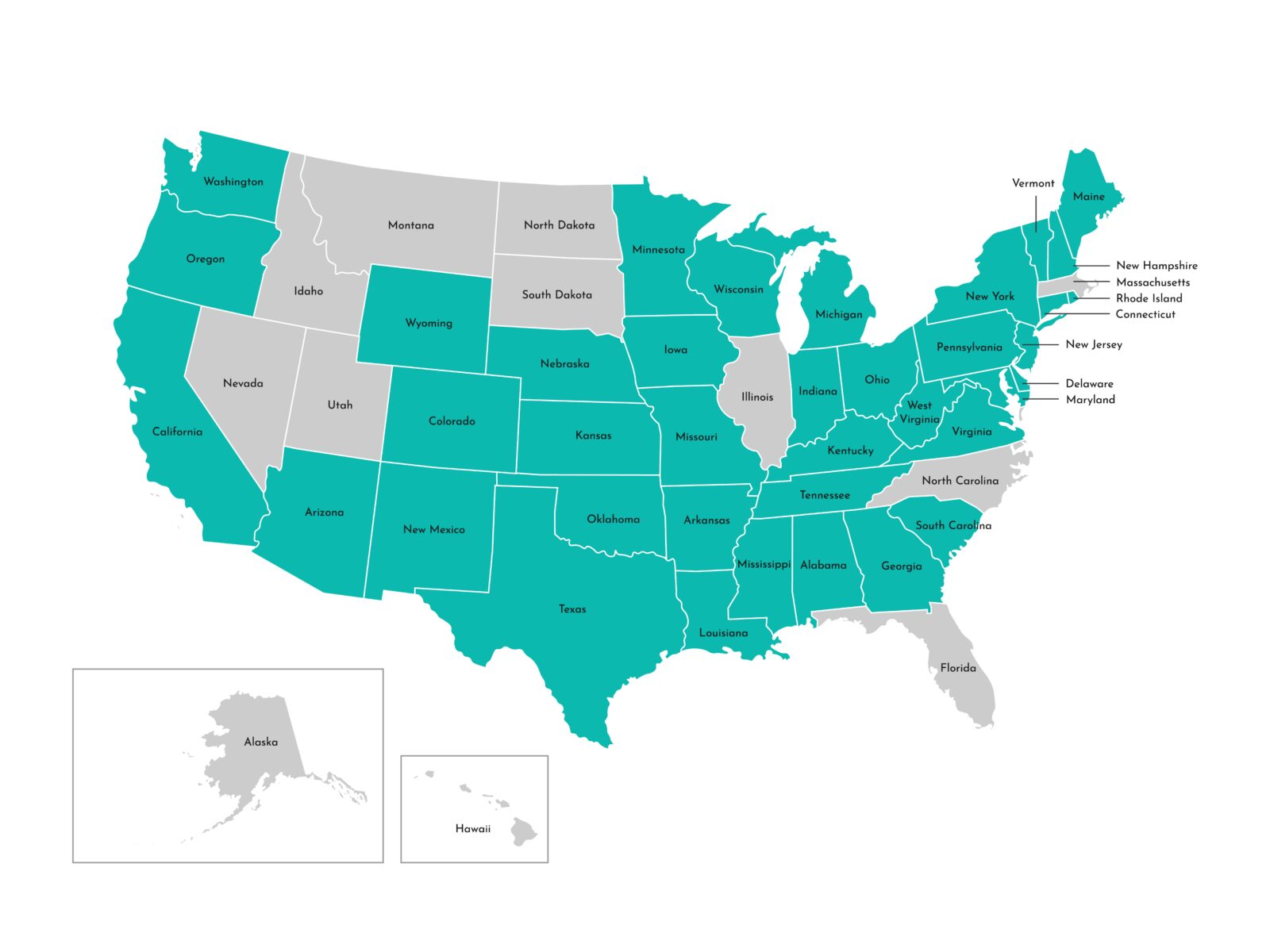
Informed Consent
Finally, there are 38 states, including the District of Columbia, that have an informed consent requirement in their administrative code, Medicaid policies or statutes. Informed consent means the patient understand the facts and risks involved with using telehealth services.
Those states are:
- Alabama
- Arizona
- Arkansas
- California
- Colorado
- Connecticut
- Delaware
- Georgia
- Idaho
- Indiana
- Kansas
- Kentucky
- Louisiana
- Maine
- Maryland
- Michigan
- Minnesota (for alcohol and abuse programs)
- Mississippi
- Missouri
- Nebraska
- New Hampshire
- New Jersey
- New Mexico
- New York
- Ohio
- Oklahoma
- Oregon (for physical therapy and community treatment)
- Pennsylvania
- Rhode Island
- South Carolina
- Tennessee
- Texas
- Vermont
- Virginia
- Washington
- West Virginia
- Wisconsin
- Wyoming
The use of telehealth isn’t as simple as simply requesting to see a healthcare provider virtually. The laws are constantly changing as the technology evolves, which can make it difficult to keep up with the latest regulations.
Fortunately, more states are getting on board with telehealth, improving access to healthcare services for patients all across the country.