Discussions involving nurse practitioners (NPs) and their role in healthcare often include terms such as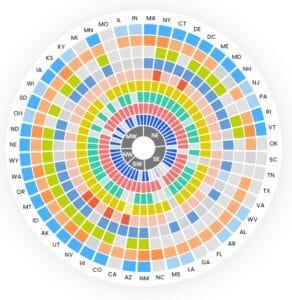
What is scope of practice for nurse practitioners?
Scope of practice is defined as the particular procedures, actions, and processes that a healthcare provider is legally permitted to do. Scope of practice varies by state according to each state’s laws. However, the American Association of Nurse Practitioners (AANP) succinctly defines a nurse practitioner’s general scope of practice and abilities:
“Nurse practitioners are licensed, independent practitioners who practice in ambulatory, acute, and long-term care as primary and/or specialty care providers. Nurse practitioners assess, diagnose, treat, and manage acute episodic and chronic illnesses. Nurse practitioners are experts in health promotion and disease prevention. They order, conduct, supervise, and interpret diagnostic and laboratory tests, prescribe pharmacological agents and nonpharmacologic therapies, as well as teach and counsel patients, among other services.”
How does scope of practice differ between registered nurses and nurse practitioners?
While the scope of practice between an NP and a physician can often be similar, the scope of practice between an NP and a registered nurse (RN) is quite different.
An RN can legally make a nursing diagnosis and implement a nursing treatment, such as health education. In contrast, depending on the state, an NP can legally make a medical diagnosis and implement treatments such as prescription medication, diagnostic imaging, and invasive procedures.
Nurse Practitioner Scope of Practice by State
Some states allow a more progressive scope of practice for NPs, while others require physicians to supervise their actions. Physician supervision laws in states such as Texas, California, and South Carolina limit the services that nurse practitioners are legally allowed to do, sometimes decreasing patient access to medical care. In contrast, states such as Washington and Maine allow NPs to provide patient care without such limitations. This Interactive Scope of Practice Law Guide illustrates scope of practice differences among states.
Despite this variation, all NPs are educated to practice as independent practitioners—that is, without physician supervision or oversight—regardless of where they attend nurse practitioner school.
What is independent practice for nurse practitioners?
Independent practice is an NP’s ability to provide care without mandated supervision from a physician. In short, it is a label given to a type of scope of practice. An NP who lives in a state that has granted independence in its scope of practice can assess, diagnose, and treat a patient in the same way that physicians do. In total, 27 states (and Washington D.C.) allow NPs to diagnose and treat patients without physician involvement.
As mentioned earlier, the degree of independence varies between states, and it is a contentious topic among national organizations representing both NPs and physicians. The AANP categorizes each state’s degree of independence as full practice (entirely independent), reduced practice (partially independent), and restricted practice (non independent).
In full practice states, NPs can provide patient care without physician involvement. In reduced practice states, laws require physicians to have some involvement, such as discussing patient cases with NPs or meeting some of their patients. In restricted practice states, laws prohibit NPs from providing care they were educated to provide and require costly supervisory agreements between NPs and physicians.
Lobbying efforts focus on achieving independence in all states as recommended by the Institute of Medicine, AARP, Robert Wood Johnson Foundation, and National Council of State Boards of Nursing. National legislation passed in 2016 granted independent practice to all NPs who work in Veterans Affairs facilities regardless of which state they are in.
What are the benefits of full practice authority for nurse practitioners?
Since NPs in full practice authority states can diagnose and treat disease without physician supervision, this opens the door for NPs to take on roles with greater responsibilities and potentially better pay. In addition, full practice authority for NPs can increase job opportunities for these crucial medical providers, since facilities can leverage their skills instead of only hiring doctors.
NPs who work in full practice authority states play a crucial role in expanding patient access to healthcare, as rural and short-staffed healthcare facilities can lean on both NPs and physicians to provide comprehensive care instead of relying solely on physicians.
Prescriptive Authority
Prescriptive authority refers to a healthcare provider’s legal ability to prescribe prescription medication. Patients and even employers often wonder, “Can NPs prescribe medication?” Or, in other words, “Do NPs have prescriptive authority?” The answer is yes, however the scope of prescriptive authority all depends on the state.
The degree to which NPs can prescribe medication without mandated physician supervision, however, varies by state. Today, in 27 states and Washington D.C., NPs have the explicit legal authority to prescribe. In the remaining states, NPs can still write prescriptions, however there is some mandated oversight from a physician.
Lobbying efforts from NP organizations also focus on removing these unnecessary legal barriers to prescribing medication. The AANP advocates for nurse practitioners’ ability to prescribe without physician involvement, that state boards of nursing (not physician state boards) be responsible for NP prescriptive authority regulation, and that nurse practitioners be able to prescribe medical devices and services such as home healthcare in addition to medication.
Campaign for Consensus
Because of the variation among states regarding what NPs can and cannot do, the National Council of State Boards of Nursing (NCSBN) launched the Campaign for Consensus, which aims to help states achieve independent practice for advanced practice registered nurses (APRNs), which includes NPs.
Moreover, the campaign aims to align individual state laws with the current best practices for healthcare regulations, licensure, education, and certification, and strives to help consumers, employers, and other healthcare providers understand the correct scope of practice for NPs.
Specifically, the Campaign lobbies for all states to incorporate these rules into their legislation:
- Recognition of the titles of the four types of APRNs.
- Licensure as both an RN and as an APRN.
- Graduate or postgraduate education from an accredited institution.
- Board-issued certification in a medical specialty.
- Independent practice.
- Independent prescribing.
ARPN vs NP: What’s the difference?
Advanced practice registered nurse (APRN) is the umbrella term for all nurses with post-graduate education and training. NPs are a type of APRN, which also includes clinical nurse specialists, certified registered nurse anesthetists (CRNAs), and certified nurse-midwives.
Learn More
This article is just the tip of the iceberg! To get involved in NP advocacy, contact your local NP organization or join the AANP. To learn more about NP scope of practice and independent practice, check out these resources:
- Our Interactive Scope of Practice Law Guide.
- Our “Can an NP Do That?” infographic.
- Dr. Carolyn Buppert’s Nurse Practitioner’s Business Practice and Legal Guide, Fifth Edition.
- AANP’s State Practice Environment map.
Become a Locum Tenens NP with Barton
Looking to travel the United States and help patients in need as an NP? Check out our job board and apply to an open position today!
Editor’s Note: This blog was originally written by Dr. Melissa De Capua, DNP, PMHNP in January 2017 and was updated by Mike Connors in April 2024 to reflect new information.


